
According to the World Health Organization, about 108 million global blood donations are collected annually. From 2013 to 2018, there has been a 7.8 million increase in blood donations from voluntary donors, yet many countries faced demands exceeding supply.
Now with lockdowns, social distancing, cancellations of blood drives, and low donor turnout, due to fears of contracting COVID-19, this shortage crisis has intensified. Normally, a significant amount of blood collections come from mobile drives at schools, universities, and employers, but collections have diminished. In India, for example, the annual requirement for units of blood is around 26.5 million, but last year only 13.5 million units were available, despite having 500 million eligible donors.
Fear of contracting COVID-19 is another reason for blood supply drops. In the Eastern Mediterranean Region, a survey with 16 blood bank medical directors from 15 Eastern Mediterranean Region countries found that representatives from 14 countries believed public fear of contracting COVID-19 contributed to decreasing donations. Concerns with exposure to COVID-19 from patients or donors has also decreased donation staff and services, lowering the blood supply.
The lack of blood donations caused by the pandemic has heavily impacted a certain health condition: β-thalassemia major.
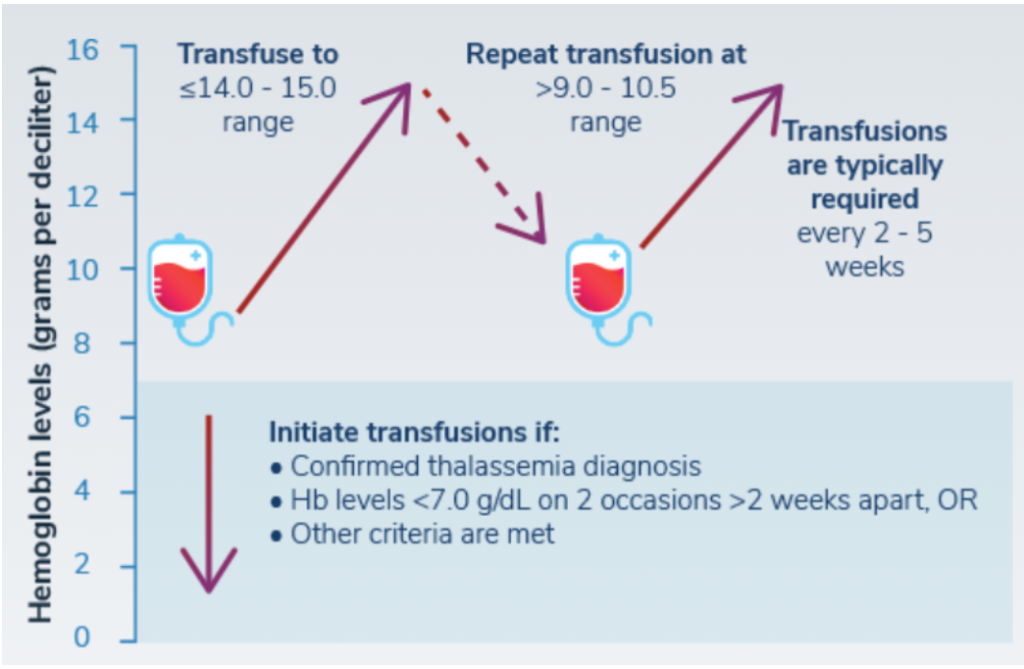
β-thalassemia major is an inherited blood disorder that results in the body producing less hemoglobin. Hemoglobin is an iron-rich protein that carries oxygen in red blood cells throughout the body. Patients with β-thalassemia major have severe anemia and need frequent blood transfusions. Since blood resources have become incredibly strained due to the pandemic, a moderate to severe drop in hemoglobin for β-thalassemia major patients has been observed. This results in numerous complications, such as growth retardation in children, worsening symptoms of enlarged organs and weakened bones, and heart failure.
Randa, a β-thalassemia major patient born in Lebanon and currently living in Canada, said, “Because of the pandemic, we had to receive blood that isn’t your blood type. I’m O positive and I had to start receiving O negative blood.” At Canadian Blood Services, donor attendance dwindled by 30%.
“Many thalassemia patients have a lot of antibodies from repeated transfusions so we usually get very strict screenings but they weren’t doing this. I had one really bad reaction with throbbing pain and a rash on my back. I wasn’t breathing normally and had high blood pressure. I’ve started going every 4 weeks, not every 3 weeks to get transfused, but some patients can’t handle the symptoms of low hemoglobin,” Randa concludes.
Patients living in developing countries have faced even more challenges. Over 80% of patients with β-thalassemia major live in developing and low-income countries from the Middle East, North Africa, and South Asia which already have limited resources.
One study found a reduction in the amount of blood bags consumed in Pakistan compared to before the pandemic. This correlates with the acute shortage of blood supply. Although the number of thalassemia patients receiving transfusions decreased, this does not indicate that they did not need them, but rather patients elected to skip their appointments, just like Randa. The decline in transfusions may also be due to governments of countries with poor healthcare systems canceling elective transfusion services without understanding the urgency of these medical situations.
In Lebanon, Randa adds, “Getting blood is much more difficult than in Canada because there is no single institution taking care of it. You search for and direct your own donor. It’s all by word of mouth. On social media, I’ve seen messages every day about the need for blood. Many thalassemia patients in Lebanon go to a thalassemia center which has its own blood bank, so they bring their relatives to give blood there.”
Lebanon, facing an ongoing financial crisis, is now dealing with the pandemic. This has worsened the financial crisis and resulted in decreased funds for healthcare and overstretched public health services. One of the main difficulties Lebanon has faced in securing blood donations during the pandemic has been road closings and general wariness of dealing with medical staff due to transmission risk. Additionally, since many donated after the Beirut explosion in August 2020, they are unable to donate again for three months, posing an even greater risk for those with rarer blood types.
How can we combat the reduced blood supply? It’s not hopeless.
The two most significant ways to increase blood donations since the onset of COVID-19 have been to ease up on requirements for donation and to encourage participation in blood drives. Most donation agencies had a minimum waiting period following certain high-risk activities. Since the COVID-19 outbreak, these requirements have been shortened and some travel restrictions have been lifted entirely. The hope is that by increasing the pool of eligible donors, these agencies will be able to meet the donation quota required to maintain proper care. Governments also need to build awareness of current safety protocols by blood collection centers to reassure the public on blood donation safety. Additionally, support needs to be extended for the safe and easy movement of donors.
Increasing awareness and education about blood donations have always been a campaign used by blood supply agencies. These projects have been heightened in the era of COVID-19 blood shortages, which have provided a rallying cry for these agencies to attract donors. Due to the shortage, blood banks have started using Facebook and their blood donation tool to contact registered donors. Bringing awareness to this Facebook feature can help reduce blood shortages by encouraging people to register to be donors who can be contacted in times of need. Efforts to increase first-time donors, such as social media campaigns targeted at young adults, are also significant as people are more likely to continue with future donations after their first donation. Increasing the number of first-time donors will ultimately lead to an increase in repeat donors who are so important for maintaining blood supplies.